The floor is being hit with a head and against the wall. Shouting in discomfort. Desperate. This is the way Josep Riba, 55, from Catalonia lived his day-to-day moments with cluster headaches. When he was 21 years old, the intense headaches were present around six, seven, or eight times daily that lasted between two and three hours. “They were like constant attacks on my brain and face. I would eventually lay on the ground like the cockroach. I was screaming and would have wanted to drown. It was hard to sleep, or remain alive,” he recalls of the most terrifying instances. Cluster headaches are uncommon, and their cause is not known. According to neurologists the pain they cause can be fatal to patients and cause deep despair and suicidal thoughts. The current treatments, ranging from high-dose corticosteroids, to Botox as well as lithium don’t always deliver results. In the most difficult instances of resistance to treatment, such as Riba’s, there is only one choice that is to implant electrodes into the brain to limit the severity of the discomfort. “Now after my operation at the very least, I will don’t have to lie on the ground or scream,” he says, in a state of resignation. He is plagued by half a dozen headaches every evening, each lasting approximately 20 minutes.
In 1939, the American physician Bayard T. Norton referred to this peculiar pain in 1939, the doctor described it as “a painful condition that was so severe that patients must be closely monitored to determine the risk of suicide.” The condition was then known as “the suicidal headache.” It’s an extremely serious problem, says Doctor. Robert Belvis, head of the Headache Unit at Hospital Sant Pau in Barcelona: “They call it due to the danger that is involved. Suicide attempts aren’t that widespread, but suicidal behaviour is. Patients have said that they would like to take themselves off something, but aren’t doing it.” Patients who suffer from this condition are monitored by suicide prevention teams of psychiatric facilities.
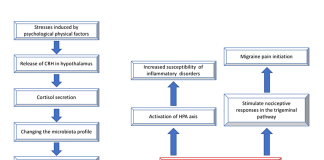
There is no way to determine what causes cluster headaches that affect 1 of every 1,000 with three times the number of males than women. Belvis says that no genetic link has been discovered and the disorder doesn’t appear to be inherited. If a patient experiences attacks, it is the hypothalamus that will be the first part of the brain that suffers but the reason is not known: “The genes of the hypothalamus are being studied due to the fact that substances known as orexins are created in the hypothalamus. The researchers have tried to determine whether there is any sort of relationship, but no connection was found”. Additionally, it’s difficult to determine the cause in emergency situations or among neurologists. In Spain the diagnosis process takes about four years on average as opposed to six years for the United States and 11 in Norway Belvis. Belvis. Each patient is unique. The majority of them suffer from attacks throughout the year, particularly during the autumn or spring months however, the majority suffer discomfort randomly, with no specific pattern. In every case, begin with an occasional ache of extreme or extreme severity (migraines however are either severe or moderate). “One morning, you begin having a series of painful attacks that last between one week to three months. It appears like you’ve hit the patient’s eye. He is crying, becomes red, his eyelids swell and the forehead expands. tears and mucus are released only on this side. The patient has the feeling that his ear is blocked,” Belvis explains. The symptoms are accompanied with agitation-related episodes The neurologist says: “There are people who begin hitting themselves, and then self-injure to prevent the discomfort. Patients usually say it’s like their eye was pulled out. It’s a serious discomfort.”
The therapeutic arsenal is huge However, it doesn’t always perform. In the event of a crisis, doctors will use triptans, the most potent family of anti-migraine medications and provide 100 percent oxygen for about half an hour (in cases of bronchitis or asthma 28% of the dose is administered for many hours). “Oxygen acts as a vasoconstrictor that stops from the creation of nitric oxide that is among the compounds which cause neuronal pain,” says the neurologist. Cortisone that is high-dose is also prescribed. Certain medications are used to reduce the severity and frequency of the attacks, including lithium (an active antipsychotic exclusively used for bipolar disorder and this condition) Antiepileptic medications, Botox injections, and an antibody monoclonal used for migraines.
10 10% of patients do not respond to any medication and need surgery. The most minimally invasive procedure is the radiofrequency of sphenopalatine nerve, which is introduced into the nerve through the mouth. It heating it and removing the discomfort. If this does not perform, neurosurgeons decide to add an Occipital nerve stimulatorthat will require an additional and more complicated procedure. Patients with chronic cluster headaches are not responsive to treatment, and the sole treatment option is deep brain stimulation.
The literature on science describes just the 94 instances that have undergone this procedure, according to Belvis. It is the Hospital Sant Pau is known for its surgical interventions. They’ve conducted 14 of them and currently conduct at least two or three every year, according to Rodrigo Rodriguez, neurosurgeon and deputy and director for the Tactical Functional Unit at Hospital Sant Pau. “The method involves the placement of an electrode in a region within the brain area that is unable to respond in a proper manner [in this instance the hypothalamus], to trigger an electrical disturbance that can alter the electrical flow of various brain structures, thereby restoring brain functioning,” he explains. The procedure is utilized frequently for other conditions like Parkinson’s.
Following this procedure the majority of patients experience improvement in their clinical condition. Like in the case of Riba headaches, headaches don’t disappear completely but they can be reduced by 50% and become less in intensity, says Rodriguez who is a neurosurgeon at Sant Pau who is also responsible for these procedures. The procedure, according to the doctor, is extremely safe and doesn’t cause any problems. He states that “the operation starts before you enter an operating area.” “There there is an abundance of planning ahead, that involves analyzing the pain circuit and determine what networks are affected. This aspect of planning is essential because it adds assurance to the process inside the surgical room.”
If neurosurgeons decide to create holes into the skull in order to insert electrodes in the hypothalamus at the base of the hypothalamus, they aim for an exact shot. Prior planning permits them to plan their precise route. By using a crown-like device which marks the spatial coordinates of the site that they want to operate, the surgeons are able to insert the electrodes. There is no room for error, however surgeons perform an in-office CT scan to ensure that the electrodes have been correctly located.
Most of the time there is a decrease in the frequency of headaches or the severity of pain decreases. There is a noticeable change in the patient’s condition prior to surgery. But, according to the surgeons that there’s always some patients who don’t respond to operation. There are no alternatives and include a variety of treatment and medications that ease headaches and provide support to patients and keep researching to discover new possibilities. A lot remains to be learned about this condition.

We understand how important it is to choose a chiropractor that is right for you. It is our belief that educating our patients is a very important part of the success we see in our offices.