As the survivor of a devastating brain injury that occurred less than 10 years ago, Heather Schroeder is no stranger to headaches. She has managed her frequent migraines by taking medications and Botox injections ever since a horse-riding accident. When she contracted COVID-19, in July 2021 the headaches she endured were “living in hell,” she says.
“Unlike migraines that are due to my TBI it was as a blanket was being placed across my forehead. It was not a matter of suffering from headaches. I had a sudden headache that was painful,” says Schroeder, 52 years old and from Knoxville, Tennessee. “A regular migraine to me is between eight and one out of 10 with nausea, light sensitivity as well as post-migraine malaise. The headache I experienced was 20 out of 10.”
There was no way that Tylenol [paracetamolor Tylenol [paracetamol] Tylenol [paracetamol]nor migraine relief medications eased discomfort, she claims. The headache lasted for two weeks, and it prevented her from sleeping, allowing just 15 to 45 minutes per day. “A majority of people I’ve met were in COVID-related quarantine, either reading or watching TV,” Schroeder says. “I had to wear the cold compress on my head, trying to get through the pain of headache.”
Schroeder isn’t alone. A recent study of research findings, around 50% of people suffering from COVID infections that were acute experienced headaches which was also the primary sign in around one quarter of the people. While COVID is classified as a respiratory disorder approximately one-in-five sufferers with moderate or severe COVID claim that it is the neurological symptoms, including headaches as well as brain fog and loss of smell and taste that affected them the most.
These percentages could be to be understated. “The report of headaches varies according to whether it’s evaluated as an outpatient or inpatient,” states Mia Tova Minen, chief of research on headaches and a neurologist at New York University Langone Health. “It’s likely to be under-reported by hospitalized patients, in part due to the fact that there’s plenty of other symptoms that could be the primary concern of these patients.”
Different types of COVID-19 headaches Types of COVID-19 headaches
A headache is typically an early COVID sign and usually occurs bilaterally either side as well as the “whole head” according to some who have described. The intensity of the pain ranges from mild to severe, but a few individuals have told National Geographic that the pain was much more severe than in prior headaches Others rated the pain as comparable with prior migraines. However, between 47 to 80 percent of those who have had an history of headaches have described their COVID headaches as distinct from their previous headaches, and with painfulness that was abrupt and intense.
Schroeder for instance, states that her migraines started slowly, which gave her time to cut down on light exposure and taking medication. However, her COVID headache started immediately and her migraines following her illness aren’t identical. “My migraines are far less manageable, and during the early spring and fall, they were more frequent than previously,” she says.
His husband Jesse Trucks, also was afflicted with an TBI from injuries sustained in sports as did his wife. He, too was vaccinated at the age of four months prior to receiving COVID-19. He also experienced a headache that was described by him as different from the ones resulting from the brain injury. “The discomfort of this COVID headache was similar to when the dentist’s drill strikes the nerve,” he says. However, while his headaches usually create a band around the top of the head, the COVID headache sat in the middle of his neck as well as the back of the head. It lasted over 10 days.
The headaches that sufferers with COVID that is acute fall into three broad categories as per Jennifer Frontera, a neurologist at the New York University’s Grossman School of Medicine. They include migraine-like tension-type and persistent headaches. Each of these are different types of headaches that exist.
A few people with COVID report headaches resembling migraines, with the head experiencing throbbing. the head. It is usually accompanied by nausea, vomiting as well as sensitivity to light and sound. Numerous studies have revealed the most frequent symptoms for COVID headaches as being similar to those seen in tension-type headaches that occur on both sides of the head and exhibit an appearance that is more “rubber band-like” restriction over your head.” Frontera says. About 70 to 80 percent of patients say they happen across both sides and on at the top of the heads and are described as having the appearance of a “pressing” or “tightening” nature. Sensitivity to sound or light, as well as nausea or vomiting On the other hand are seen within less than half people suffering from COVID headaches.
However, some COVID-related tension-type headaches are also characterized by another characteristic which warrants a third classification which is that they can are persistent for days, weeks and sometimes even for months. They are similar to “new daily , persistent headaches,” a diagnosis for a headache that won’t stop and can be triggered by an infection that is viral or medical procedure an event in life that is stressful or even a flight, Minen says. While it is only officially diagnosed as a new, persistent headache after a period of up to 90 day, Minen states that doctors generally recognize these headaches and can start treating them earlier.
Daily, frequent headaches might not be as sensitive to standard treatments for migraines or the more traditional tension-type headaches that has led some headache specialists to couple them with the persistent headaches that sufferers experience during COVID-related episodes, Minen says.
In one study of over 90 COVID patients, their headaches averaged 14 days. However, one-in-five patients was suffering from it three months later. Another of six patients experienced it nine months after. The more severe the headache in the acute phase and the longer they were more likely to experience headaches.
The causes of COVID-19 headaches
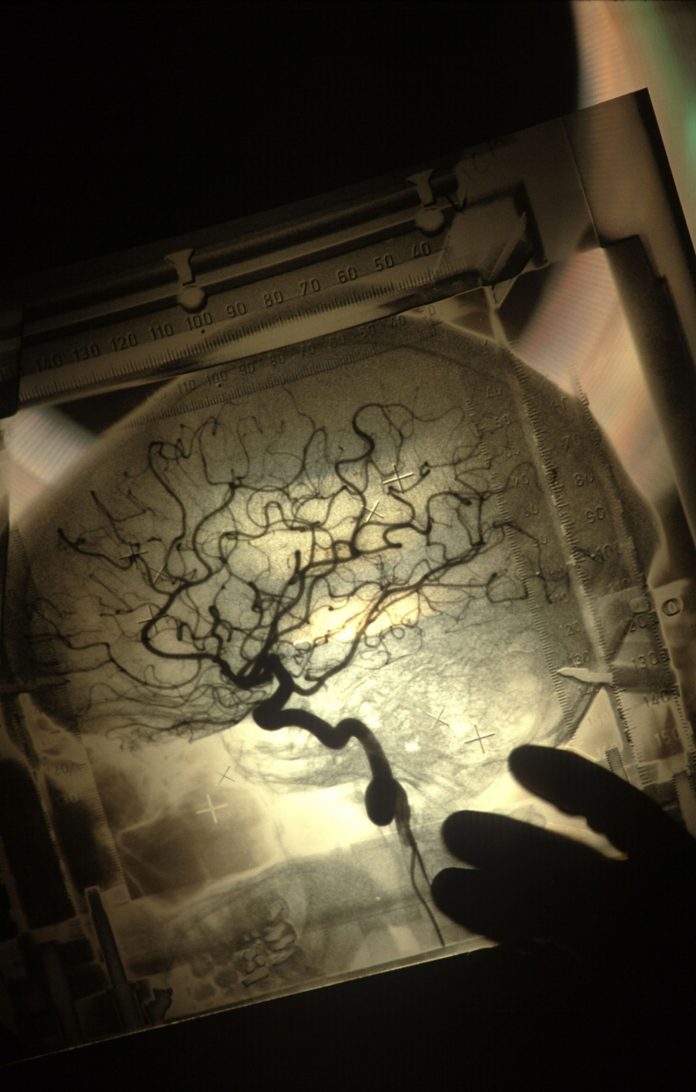
Researchers are still trying to discover the precise mechanisms that cause COVID-19 headache. However, some possible causes include direct damage caused by COVID, an reaction to inflammation in the body as it fights off the virus, less oxygen in blood, dehydration, issues with blood clotting or problems with the endothelial cells which create the blood vessels. None of these could, however, can explain the cause of all COVID headaches.
“There’s likely to be a few different mechanisms in play,” Frontera says. “The most persuasive pathological evidence refers to microvascular damage,” she says. Negative effects caused by COVID-19 to blood vessels are acknowledged and can impact the trigeminal nerve which is the biggest cerebellar nerve that is that is responsible for facial sensations as well as motor actions, like eating and swallowing. It is located near the temple just in the front of the ear on the opposite side from the forehead, each trigeminal nerve ganglion — a group of nerves that has three branches running along both the upper, middle and bottom of the face.
“There’s an relationship between headaches and loss of of smell and taste which means that one of the possible causes could be due to something wrong with this olfactory pathway” Minen says. “It may be because COVID is entering the nose and causing inflammation of the nasal cavities. Then, Trigeminal nerve branches that can result in headaches.”
Laura Johansen, a public health clinical researcher from Charlotte, North Carolina, discovered that her headache after suffering from COVID-19 in October of 2020 “aligned nearly perfectly with the time I began losing my sense of smell and taste and increased with each other,” a common association in study. As with many COVID headaches Hers was concentrated in the front and the top of her head.
“It was like a sinus migraine that became an attack of migraine” Johansen says. “It was for about four days. When it started to manifest the body, it was firmly parked. No flow or ebbs or aches that lasted for a long time.” While she did take Acetaminophen, she says it didn’t help much.
Acetaminophen is also commonly referred to as paracetamol in the UK is among the most popular treatments doctors prescribe along with non-steroidal anti-inflammatory medicines, triptans, metamizole, or a combination of them but only about 25% of patients experience complete relief. Only half of them reported any relief from these medicines. Minen claims that specialists for headaches will typically deal with tension headaches or constant daily headaches by using gabapentin, an anti-inflammatory medication also used to treat seizures as well as nerve pain.
“Certainly If you’re not responding to the basic non-prescription painkillers It’s likely to be a good idea to schedule the appointment to see a specialist in headaches,” Frontera says. “One is to ensure there’s nothing other than normal as well as to determine the type of headache you’re experiencing.” Treatments differ for migraine-like headaches as opposed to tension-type or chronic headaches according to Frontera.
Long COVID headaches
While COVID-related headaches are relieved by other signs in the majority of individuals, up to 45 percent of sufferers are still suffering from headaches when other symptoms have diminished.
Travis Littlechilds Systems analyst, living in London and has been suffering from COVID headache on a daily basis over the last four months. The pain during active inflammation was similar to migraine according to him, “but extra sensitive to pressure.” The act of bending over or coughing caused a lot of pain. While his headaches are less frequent however their intensity is similar: a strong pressure on his back of the head which is more painful when moving.
Other patients with chronic COVID have reported the headache that they experienced as a result of the infection lasted for a long time. A meta-analysis of 36 studies that involved more than 28,000 patients suffering from COVID, headaches lasted for as long as two months for one out of six individuals and as long as 3 months in the case of one person in 10. In 8 percent of the patients the headache lasted for at the very least for six months. The majority of studies on COVID headaches does not address the question of the difference in symptoms between those who have been vaccinated or not however, a recent study revealed that for those vaccination- or booster-vaccinated, headaches were among the more mild symptoms.
People most likely to experience an extended COVID headache are those who have an history of headaches and who had headaches as the first symptom, and whose COVID headache was more severe than other COVID symptoms, or who did not respond to pain medication. Patients with COVID post-covid headaches tend to respond well to migraine medication amitriptyline or nortriptyline Frontera says.
Schroeder who’s illness was primarily a fatigue and headache, without symptoms of chest tightness or sniffles. was blessed not to suffer an extended COVID headache and she as well as her husband continue to be on guard to prevent a second infection.
“I will never experience a headache that bad ever again,” she says. “I take a look back and think about what I did to survive the event. It’s odd that I don’t remember the events well … however, I do remember the agony completely.”

We understand how important it is to choose a chiropractor that is right for you. It is our belief that educating our patients is a very important part of the success we see in our offices.