Two different approaches to conservative treatment are effective in treating subacute and acute spine pain New research suggests.
The results of studies like the SPINE CARE randomized controlled study revealed that 6-8 weeks of individualized postural rehabilitation (IPT) or a multidisciplinary biopsychosocial treatment called ICE which includes physical therapy, were linked to small, yet statistically meaningful reductions of disability due to pain after 3 months, compared to regular care.
Additionally, the spine-related health care expenditures was not much different between ICE and regular treatment. But, IPT significantly increased spending in comparison to normal treatment.
Dr. Niteesh Choudhry
“We observed that, in comparison to standard primary treatment, both interventions decreased the disability associated with pain by 3 months. These improvements lasted and were clinically significant at 12 months even after the interventions were completed,” lead author Niteesh K. Choudhry, MD, PhD, Brigham and Women’s Hospital and Harvard Medical School in Boston, Massachusetts, told Medscape Medical News.
The results were released online the 20th of December by JAMA.
Common Complaint
Spine pain refers to discomfort that is felt either in your neck or back The researchers note. It “accounted for the most health-related expenditure than any other health issue on the US in 2016” they say.
“Spine pain is a frequent reason for patients to visit their primary healthcare providers,” Choudhry said.
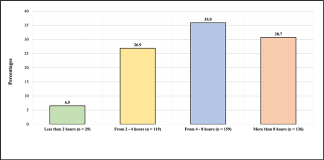
It was the SPINE CARE trial included 2971 adult participants (60 percent females; mean age 51 years) suffering from back and neck pain lasting shorter than twelve weeks. The participants were randomly assigned to standard treatment (no intervention or treatment, 992) or to ICE (n 829) or IPT (n 1150) interventions.
It is the “identify the cause, plan, and improve” (ICE) treatment model divides patients based on their likelihood of progressing from chronic to acute pain. It also addresses the biopsychosocial factors that contribute to pain. Patients at low risk got only one session of physical therapy (PT) visit as well as one coaching session, whereas those at higher risk were provided with three PT visits as well as three coaching calls and one electronic consultation.
The IPT intervention that was offered in 8 weekly sessions, is focused on postural alignment. IPT is also focused on self-efficacy as well as self-management. It includes daily exercises that improve coordination, postural control and balance.
The results at 3 months revealed that both ICE or IPT groups had significantly better results than the IPT group in Oswestry Disability Index (ODI) scores than the standard care group.
| Intervention | Mean ODI changes to three months |
|---|---|
| ICE | 31.2 to 15.4 |
| IPT | 29.3 to 15.4 |
| Usual care | 28.9 to 19.5 |
At three months, the change in ODI score vs . usual treatment measured -5.8 to be exact for ICE (95 percent of the CI, -7.7 to -3.9; P > .001) as well as -4.3 in the case of IPT (95 percent IPT CI, -5.9 to -2.6; P .001) to IPT.
Both interventions decreased the use of resources for diagnosis imaging procedures and doctor visits, Choudhry reported. “Because these interventions, they interventions reduced expenditure not directly related to the interventions,” he added.
If the costs of intervention are included ICE was associated with lower expenses overall than normal treatment ($139 less) and overall expenses for IPT was higher than typical treatment (by 941 dollars).
“We evaluated intervention strategies in a manner that were implemented in primary healthcare, which means the implementation in other settings of practice is not difficult,” Choudhry said.
He also pointed out the ICE model doesn’t currently exist as a full program however, its components, like physical therapy and specialist e-consults do. “And we believe that our findings warrant looking at ways to implement this in a more general way,” he said.
Choudhry stated that IPT was evaluated using an individual service (Egoscue), “which has various locations across locations in the US and around the world, it should be simple to incorporate into daily practice.”
However, other crucial elements, such as insurance coverage, need to be examined in the near future the minister added.
Do you have evidence to support it?
In the accompanying editorial Erin Krebs, MD, Minneapolis VA Health Care System, Minnesota, and colleagues mention that prior systematic studies have found that exercise-based therapies are “generally efficient” to treat chronic back and neck pain that is typically described as pain lasting longer than 12 weeks however, they are not effective for acute pain. This is defined as pain lasting between 4 to 6 weeks.
“The current study provides evidence of the efficacy of exercise therapy in patients who are experiencing an episode that is under 12 weeks. This means that they are not chronic yet but not necessarily severe,” the editorialists write.
“Clinicians will more often suggest exercises that are structured for those suffering from the subacute back and neck discomfort, particularly if the pain is persistent,” they add.
The study was financed by unrestricted philanthropic donations towards Stanford University. Choudhry was awarded grants from Stanford University during the conduct of the research. The complete list of disclosures for editors and researchers is provided in the original report.
JAMA. The journal was published online on 20th December in 2022. Abstract, Editorial
To get additional Medscape Neurology news, join us on Facebook and Twitter.

We understand how important it is to choose a chiropractor that is right for you. It is our belief that educating our patients is a very important part of the success we see in our offices.