The foot and hip pain as well as the connection between hyperpronation and sciatic pain.
The term “SCIATICA” is a description of a set of symptoms not a diagnosis according to Janet Travell, MD, the pioneer of trigger point therapy, outlined in the classic Trigger Point Manual. One of the biggest problems is that searching the internet for the word “sciatica diagnosis” will show an array of contradicting views among medical professionals as well as the link between foot and hip pain. The majority of them believe that sciatica is a sign of a deterioration or a deterioration of sciatic nerve as a result of a radiculopathy or an entrapment which is, that is, an indication of illness or injury.
Injury-centric
My name for this prevalent perspective refers to “injury-centric” mentality. This belief holds that pain is caused by injuries or diseases within the physical structures like joints and nerves, tendons, or nerves. bursa, which is usually close to the location of the perceived pain.
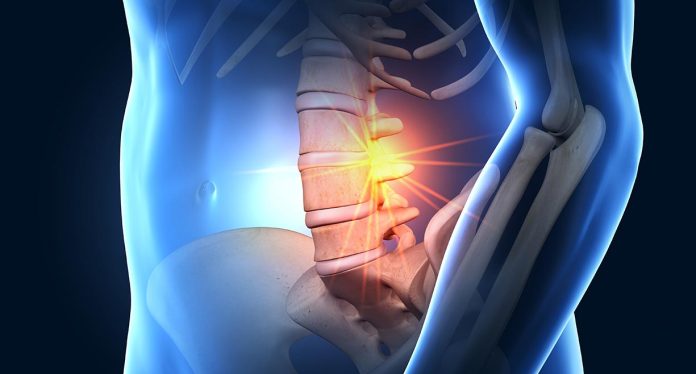
Radiating pain , as observed in sciatica is usually attributed to entrapment or impingement of the sciatic nerve or injuries to other parts of the IT band. The theory is that pain originates from the injury and pain signals are transmitted through the injury as inward signal for the brainor, in other words it can be described as an “outside-in” experience.
Modern neuroscience has thoroughly disproved this theory, but it is still prevalent in our medical system as well as popular culture. V.S. Ramachandran’s research on the phantom of limb pain is extremely instructive to understand the root of pain. Phantom limb pain is experienced as if it’s an limb that has been removed. He discovered that by using the mirror box that reflect the limb that is present to the other part of your body the evidence that is visible that the missing part being present can stop the pain in many instances. According to Ramachandran it is an outcome it is not an input.
Lorimer Mosely, PhD, collaborated with Ramachandran on his phantom-limb research and has emerged as a leading voice in the field of modern neuroscience. Mosely states the fact that “soft tissue damage isn’t essential nor sufficient for the sensation of pain.”[3The brain does not detect pain signals, it is able to detect the nociceptive (danger) signals coming from the peripheral region and decides “is this really dangerous?”
Pain is often thought of as a signal from the brain that focus must be given to the perceived injury. In some instances there’s a genuine damage or physiological problem that is setting up nociception . But these instances are very rare and a more common source of nociceptive is trigger points within muscles.
Trigger points and nocicept
Travell’s research provided numerous examples of muscles that typically create trigger points, and whose referral patterns mirror the majority of the symptoms associated with Sciatic nerve. Our research has revealed that sciatic pain usually has its roots in muscles that have trigger points. [4]
Jay Shah, MD, of the National Institutes of Health has demonstrated convincingly that trigger points can be effective sources of nociceptive signals. In addition, he introduced microtubules in the trigger point and removed the ambient fluid discovering that it contained numerous similar nociceptive compounds that can be observed in the area of tissue damage. However, trigger points aren’t injury-related and can be treated quite quickly. They are most likely to develop in situations of chronic or acute use, which may strain the local metabolism and vascular exchange, which can result in the formation of trigger points.
The concept of pain referral can be an ambiguous phenomenon that can be observed whenever trigger point are active to go over the threshold and cause an unpleasant sensation that is usually far away from the point where the trigger points are. In their study, Travell and Simons documented the direct referential patterns of a broad range of muscles. For instance trigger points within the gluteus minimus may cause the entire or a portion of a pattern of pain which includes sacral and gluteal pain, which can be felt throughout the lateral or posterior leg, as far as the ankle and foot. Because of its resemblance with the dermatomal axis of the sciatic nerve and the recurrent pattern of foot and hip pain is commonly thought to be radiculopathy or an entrapment from the nerve.
However, gluteus minimus sciatic referral is such a common phenomenon that Travell and Simons nicknamed this muscle “Pseudo-sciatica.”[6] Gluteus medius is commonly co-involved, potentially adding low back referral to the mix.
Foot and hip pain The pain of the muscles is a chain
A direct and simple transfer from one muscle is extremely rareMore frequently, a report of pain includes a variety of muscles. Certain muscles operate in a silent manner and contribute to the patterns of satellite referral where the pattern of referral for one muscle is mirrored by the trigger point from another muscles, which causes it to create the trigger point of its own. The chains may be several muscles long. Patients may only experience the insertion of the final muscle within the chain.
Although satellite referral may sound a bit cryptic and confusing, it’s an actual thing which we have discovered to be extremely significant over the course of the 20 years of clinical experience. Satellite chains were not described in the trigger point literature. However, the authors did note and discuss the phenomenon in isolated instances. We’ve also observed many frequent patterns that cause several of the most frequent symptoms of pain seen in medical practice.
Sciatic pain is the most prominent illustration. The gluteus minimus muscle pattern connects numerous muscles while it moves through the leg, including the quadriceps, hamstrings adductor magnus as well as many other muscles in the leg’s lower. While it may be tempting for practitioners to concentrate on areas of tenderness within one of the muscles that are terminal, such as vastus lateralis, it can be a major unnecessary use of time when the vastus lateralis muscle is being established by satellite re-connection through the gluteus minimus.
Alongside the existence of satellite chains, functional interactions between muscles should also be taken into consideration when determining the root of the pain. The CNS continuously monitors the connections between muscles and their antagonists, so that it can create seamless, coordinated movement at every joint. Because of this close coordination trigger point dysfunction muscles can cause dysfunction in the antagonists.
A physiotherapist and author Leon Chaitow pointed out that taut fibers that are seen in muscles that have trigger points might play an important function in that taut fibres are full contractures of the individual fiber bundles. They can also mimic the stability that is normally offered by connective tissue and ligaments. 7. It is my assumption that the CNS could introduce taut fibers to provide stability to joints that are believed as unstable because of factors like excessive muscle movement or imbalance.
One of our approaches to treating patients involves “hack to the CNS,” downregulating it by a variety of methods of neurological distraction, and allowing the experience of motion pain-free region that has been stretched by taut fibers in opposing muscles.
The length of the leg and Hyperpronation
The ankle hyperpronation is basically a failure ensure adequate stability of the foot and ankle due to ligaments that are stretched. We have seen this problem to be prevalent in twenty years of clinical practice and has been observed in particular in patients with sciatic pain.
A subtalar joint that is too mobile tends to permit the knee and femur to move valgus in a downward direction due to the an arch that is collapsed. The leg abductors including gluteals and TFL are the main way to stop the valgus’s movement by bracing the legs with abduction. The constant over-engagement of the muscles in gait is the ideal setting for creating trigger points. This can result in a recurring referral pattern that could be accompanied by the various symptoms of sciatica such as lower back sacral and gluteal discomfort and radiating to the lower leg.
Leg length discrepancies that are effective usually are associated with hyperpronation. This is especially true in cases where the pronation level differs on both sides. The quadratus lumborum as well as the iliocostalis muscle are particularly sensitive to LLD. A sacrum tilted to the side results in various lengths of resting between the two QLs and the CNS dislikes this type of discord.
The result could cause point development in either QL as a means of stabilizing an incredibly dangerous situation. The QL is a large referral pattern that includes gluteal, sacral, abdominal and radiating parts and is a potent recipe for a series of satellite referrals through the QL to the glutes and finally up to your leg. Unilateral sciatica is a typical symptom. [8]
A method for treating sciatic pain.
Our method for treating sciatic pain is based on movement-oriented bodywork to restore the muscles that are located along the satellite connection and to strengthen the functional foot and hip pain chains. This is followed by the assessment and correction hyperpronation by midfoot and forefoot support.
In the event that an efficient LLD is found the appropriate lift should be added on the shorter side, after correction of hyperpronation. These steps to correct gait are essential to ensure lasting relief. This method has proven to be extremely effective and has a high percentage of success when dealing with what could be a severe and debilitating pain syndrome.
CHUCK DUFFfounded the Coaching The Body(r) (CTB) Institute in 2001. Since then, he trained thousands of pupils in efficient techniques to ease discomfort. CTB incorporates trigger-point therapy, techniques that are based on movement which are based on traditional Thai bodywork, as well as other techniques in conjunction with the latest research from neuroscience. The workbook, Ending Pain: Coaching the Body using Neuroscience Movement, CTB, and Trigger Point Therapyis scheduled to be published in the late part of September 2022. For more details, go to coachingthebody.com.
References
1. Travell and Simons, Myofascial Dysfunction and Pain, 171.
[22 Doidge, The Brain That Changes Itself, 142.
3 “50 Shades of Pain” with Professor. Lorimer Moseley Trust Me, I’m a Physical Therapist.”
[4] Duff, Charles, Ending Pain, 223.
5 Shah and co., “Biochemicals Associated With Inflammation and Pain Are Increased in the areas that are near to and afar from active Myofascial Triggers.”
6. Travell and Simons, Myofascial Dysfunction and Pain, 1886.
[77 Chaitow, “Might Trigger Points Sometimes be useful? – Leon Chaitow.”
[8] Duff, Charles, Ending Pain, 127.
Related Posts

We understand how important it is to choose a chiropractor that is right for you. It is our belief that educating our patients is a very important part of the success we see in our offices.