Back Pain
Understanding and Treating a Herniated Disc: Your Guide to Relief and Recovery

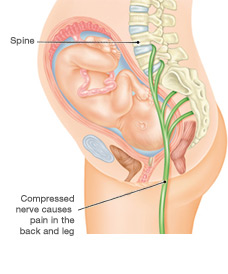
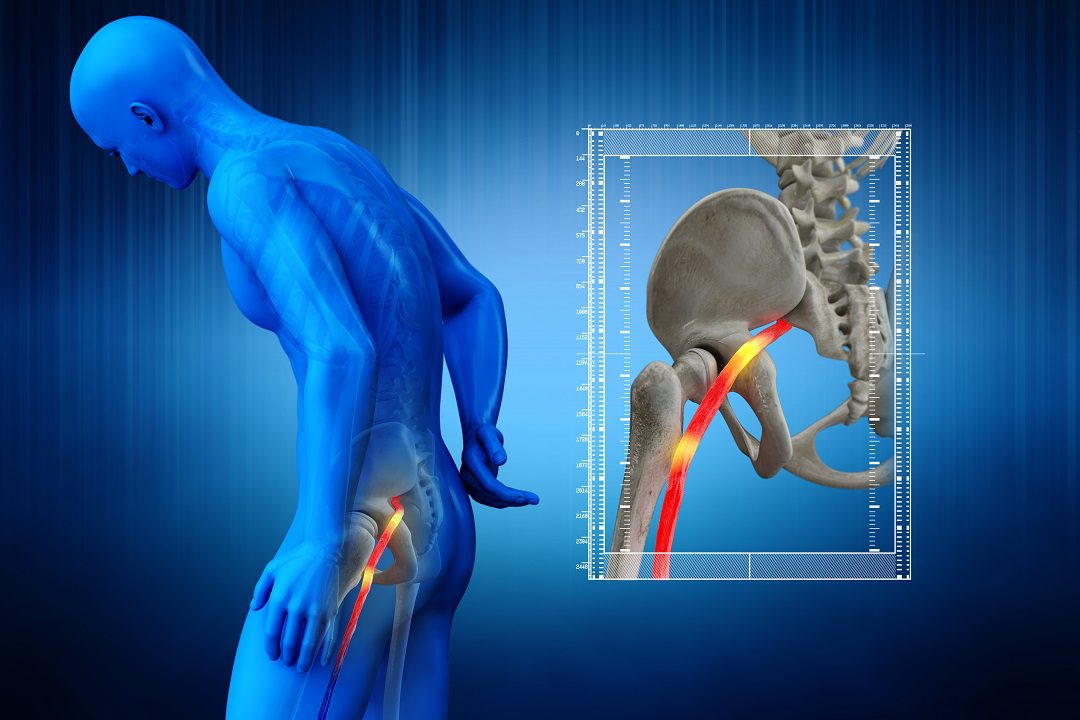
Experiencing persistent back pain or radiating discomfort down your leg can be alarming and disruptive to your daily life. Often, these challenging symptoms point to a common spinal condition: a herniated disc.
This issue is a frequent underlying cause of both sciatica and radiculopathy, terms that describe nerve-related pain originating from the spine. Understanding what a herniated disc is, how it develops, and the wide array of available treatments is crucial for effective pain management and restoring your quality of life.
This guide aims to demystify the complexities surrounding herniated discs, helping you navigate your path to relief and recovery.
Read More About Understanding and Treating a Herniated Disc
The Anatomy of Your Spine and Discs
To truly grasp what a herniated disc entails, it’s helpful to begin with a basic understanding of your spinal anatomy.
Your spine, often referred to as your spinal column or backbone, is a remarkable structure composed of 33 individual bones called vertebrae. These vertebrae are stacked one upon another, forming a protective column for your spinal cord.
The spine is divided into three main regions: the cervical spine (your neck), the thoracic spine (your mid-back), and the lumbar spine (your lower back, also known as the lumbar region).
Between most of these vertebrae are flexible, cushion-like structures known as intervertebral discs, or simply spinal discs.
Each intervertebral disc is ingeniously designed with two main parts: a tough, fibrous outer ring called the annulus fibrosus and a soft, gel-like inner core called the nucleus pulposus.
These discs serve a vital purpose, acting as shock absorbers for the spine, allowing for flexibility, and enabling smooth movement while protecting the vertebrae from impact.
Exiting from the spinal cord at each vertebral level are delicate nerve roots. These spinal nerves branch out through small openings in the vertebrae called foramen, extending to supply sensation and movement to various parts of your body, including your arms, legs, and torso.
When these vital nerve roots become compressed or irritated, that’s when problems like a herniated disc can lead to significant discomfort. Supporting this intricate structure are various ligaments, muscles, and bone components, all contributing to overall spine health.
More Things to Know About Understanding and Treating a Herniated Disc
What Causes a Herniated Disc?
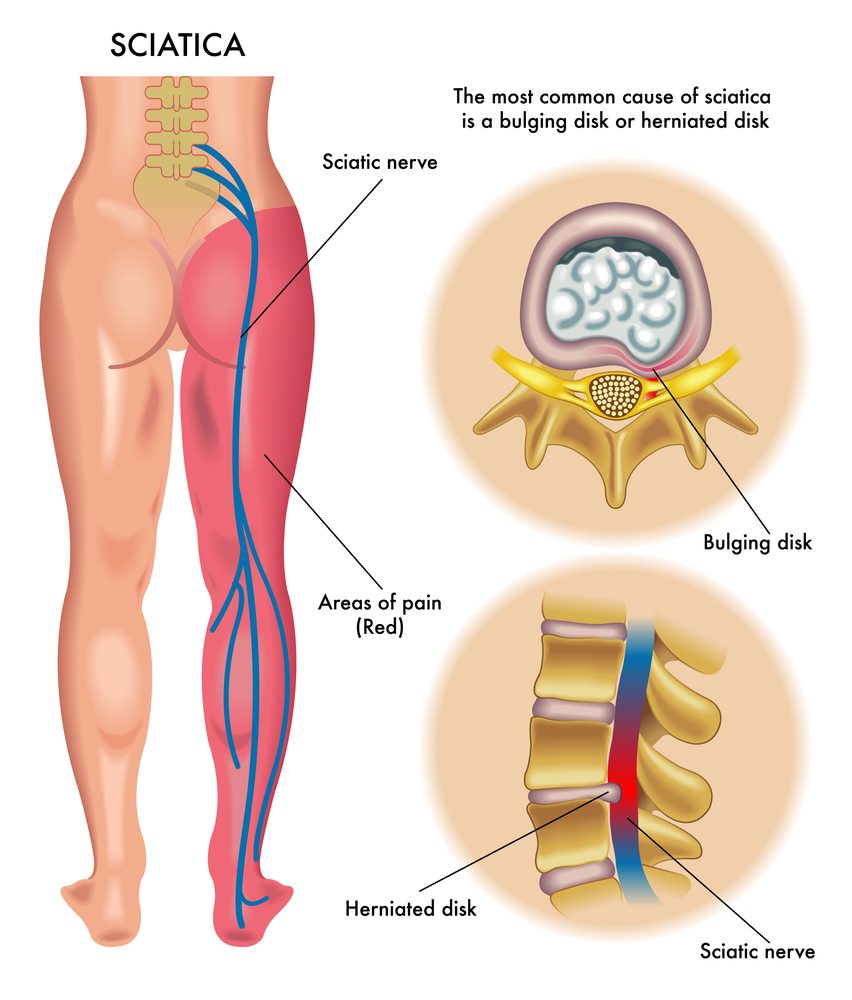
A herniated disc occurs when the soft nucleus pulposus pushes out through a tear or weakness in the tougher annulus fibrosus.
This can happen gradually over time or suddenly due to injury. The process often begins with disc degeneration, a natural aging process where the intervertebral disc loses water content and elasticity, becoming less resilient. This is a key component of degenerative disc disease, which can predispose individuals to disc problems.
When the inner material starts to push outwards, it can manifest in different stages:
- A disc bulge is when the disc pushes out uniformly around its circumference.
- A disc protrusion is a more localized bulge where the disc material extends beyond its normal boundary but the outer annulus fibrosus is still largely intact.
- A disc extrusion occurs when the nucleus pulposus breaks through the annulus fibrosus but remains connected to the disc.
- In severe cases, a disc sequestration happens when a piece of the disc breaks off entirely from the main disc.
These conditions are often colloquially referred to as a slipped disc, bulging disc, or ruptured disc.
Regardless of the specific term used, the critical issue arises when the displaced disc material causes nerve compression or nerve impingement on a nearby spinal nerve root or even the spinal cord itself, particularly in cases of spinal cord compression.
The location of the herniation determines the type of symptoms you experience:
- A lumbar disc herniation (lumbar herniated disc) in the lower back is the most common, often leading to lower back pain and sciatica (pain radiating down the leg).
- A cervical disc herniation (cervical herniated disc) in the neck can cause neck pain and symptoms radiating into the arm.
- Less commonly, a thoracic disc herniation (thoracic herniated disc) in the mid-back can cause pain that wraps around the chest or abdomen.
Other contributing factors to herniated disc causes can include poor posture, improper lifting techniques, and repetitive motions that strain the spine.
Conditions like spinal stenosis (narrowing of the spinal canal) or foraminal narrowing (narrowing of the nerve root exit points) can also exacerbate nerve compression in the presence of a herniated disc.
Recognizing Herniated Disc Symptoms
The symptoms of a herniated disc can vary widely depending on the location and severity of the herniation and which nerve root is affected. These are often described as herniation symptoms or herniated disc symptoms.
The most prominent symptom is pain. This is typically radicular pain, meaning it radiates along the path of the compressed nerve.
For a lumbar disc herniation, this manifests as leg pain, often extending from the buttocks down the back of the thigh and into the calf or foot, which is characteristic of sciatic pain.
For a cervical disc herniation, you might experience arm pain radiating from the neck into the shoulder, arm, hand, or fingers. The pain can range from a dull ache to a sharp, burning sensation, and it can be acute pain or develop into chronic pain.
Beyond pain, neurological symptoms are common indicators of nerve involvement:
- Numbness: A loss of sensation in the affected area.
- Tingling: A “pins and needles” sensation, often accompanying numbness.
- Muscle weakness: Difficulty moving or controlling muscles in the affected limb. In severe cases of lumbar herniation, this can lead to foot drop, where you struggle to lift the front part of your foot.
- Muscle spasms: Involuntary contractions of muscles near the affected area, often in the back or neck.
It’s important to distinguish these symptoms from general back pain or discogenic pain, which originates from the disc itself without direct nerve compression.
Diagnosing a Herniated Disc
If you suspect you have a herniated disc or are experiencing persistent back pain with radiating symptoms, seeking professional medical advice is essential. A thorough diagnosis is the first step toward effective treatment.
The diagnostic process typically begins with a comprehensive clinical evaluation by a healthcare professional, such as a neurologist, orthopedic specialist, or spine specialist.
They will conduct a detailed neurological examination, assessing your reflexes, muscle strength, sensation, and range of motion. They will also take a thorough medical history, asking about the nature, onset, and progression of your symptoms.
To confirm the diagnosis and pinpoint the exact location and severity of the nerve compression, imaging studies are crucial:
- Magnetic Resonance Imaging (MRI), often referred to as an MRI scan or simply MRI, is considered the gold standard. It provides highly detailed images of soft tissues like discs, nerves, and the spinal cord, making it excellent for detecting disc herniation, spinal stenosis, and nerve impingement.
- A Computed Tomography (CT) scan, or CT scan, uses X-rays to create cross-sectional images, offering good detail of bone structures. It can be used if an MRI is contraindicated or to assess bony narrowing of the spinal canal or foramen.
- An X-ray might be used initially to rule out other conditions or assess spinal alignment, though it doesn’t directly show discs or nerves.
- In some specific cases, a discography might be performed, though it is less common.
Treatment and Management: Finding Relief
The good news is that the vast majority of herniated disc cases respond well to non-surgical treatment, often referred to as conservative treatment. The primary goals are to reduce pain, improve function, and prevent recurrence.
A. Non-Surgical Approaches (Conservative Management)
- Rest and Activity Modification: In the initial acute phase, a period of rest and activity modification is often recommended to avoid aggravating the nerve. However, prolonged bed rest is generally discouraged.
- Physical Therapy and Exercise: This is a cornerstone of herniated disc treatment and herniated disc recovery. A qualified physical therapist (or physiotherapist) will design a personalized exercise regimen that includes stretching exercises to improve flexibility, core strengthening exercises to support the spine, and other rehabilitation exercises aimed at improving posture, strengthening supporting muscles, and reducing pressure on the nerve root. Exercise therapy is critical for long-term spine health and preventing future episodes. You might also be taught herniated disc exercises to do at home.
- Pain Management Techniques:
- Medications: Over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are often the first line of defense for reducing inflammation and pain. Prescription anti-inflammatory medication or muscle relaxants might also be prescribed for more severe pain or muscle spasms.
- Injections: For more targeted pain relief, corticosteroid injections can be highly effective. An epidural steroid injection (or epidural injection, cortisone injections) involves injecting anti-inflammatory medication directly into the epidural space around the spinal nerve root to reduce inflammation and pain.
- Complementary Therapies: Some individuals find relief through therapies like acupuncture or massage therapy, which can help alleviate muscle tension and promote relaxation. Traction treatment may also be considered in some cases.
- Chiropractic Care: Many individuals seek chiropractic care or chiropractic treatment from a qualified chiropractor. These practitioners focus on spinal adjustments and manipulations to improve spinal alignment and reduce nerve irritation.
- Lifestyle Modifications: Implementing posture correction and ergonomic adjustments in your daily life, especially at work, can significantly reduce stress on your spine and help prevent recurrence. A back brace might be used for temporary support in some situations.
B. Surgical Options (Surgical Intervention)
While most cases improve with conservative care, surgery may be considered if non-surgical treatments fail to provide adequate pain relief after several weeks or months, or if there is progressive muscle weakness or other severe neurological deficits (such as loss of bowel or bladder control, which is a medical emergency).
The decision for surgical intervention is typically made in consultation with a neurosurgeon or an orthopedic surgeon (orthopedic specialist), who are experts in spinal surgery (spine surgery or back surgery). Common surgery options include:
- Discectomy or microdiscectomy: This is the most common surgical procedure for a herniated disc. It involves removing the herniated portion of the disc that is pressing on the nerve. A microdiscectomy is a minimally invasive approach using a microscope for a smaller incision and faster recovery.
- Laminectomy: This procedure involves removing a portion of the vertebral bone (lamina) to create more space for the spinal cord or nerve roots, often performed in conjunction with a discectomy, especially for spinal stenosis.
- Spinal fusion: In some cases, particularly if there’s spinal instability or severe degenerative disc disease, spinal fusion may be recommended. This procedure involves permanently joining two or more vertebrae together to stabilize that segment of the spine.
- Disc replacement or disc replacement surgery: For certain patients, replacing the damaged disc with an artificial one may be an option to maintain spinal motion.
These procedures are considered orthopedic surgery or neurosurgery, depending on the specialty of the operating doctor. Advances in minimally invasive surgery (minimally invasive spine surgery) have made recovery faster and less painful for many patients. Post-surgery, rehabilitation is crucial to regain strength and function.
Prevention and Long-Term Spine Health
Preventing a herniated disc involves maintaining optimal spinal health. This includes regular exercise to keep your back strong and flexible, practicing good posture correction, and using proper body mechanics when lifting heavy objects.
A well-conditioned back with strong core muscles contributes to a stable spine and unrestricted motion, promoting stress-free movement and a harmonious alignment. Aim for a balanced posture and an exercise regimen that supports a flexible spine.
By taking these steps, you can help ensure you have a healthy disc, an intact disc, and a normal spine that remains symptom-free and pain-free.
Dealing With A Herniated Disc
A herniated disc can be a source of significant discomfort, leading to conditions like sciatica and radiculopathy. However, with a clear understanding of its causes, symptoms, and the wide range of diagnostic tools and treatment options available, you can effectively manage the condition and achieve pain relief.
Whether through comprehensive physical therapy, targeted pain management techniques, or, in some cases, surgical intervention, the path to recovery is often successful. Remember, accurate diagnosis and a tailored treatment plan are paramount.
Don’t hesitate to consult with a spine specialist or your healthcare provider to discuss your symptoms and embark on your journey toward a healthier, more comfortable life.