Sciatica
Full endoscopic versus open discectomy for sciatica: randomised controlled non-inferiority trial – The BMJ
Abstract
Objective To assess whether percutaneous transforaminal endoscopic discectomy (PTED) is non-inferior to conventional open microdiscectomy in reduction of leg pain caused by lumbar disc herniation.
Design Multicentre randomised controlled trial with non-inferiority design.
Setting Four hospitals in the Netherlands.
Participants 613 patients aged 18-70 years with at least six weeks of radiating leg pain caused by lumbar disc herniation. The trial included a predetermined set of 125 patients receiving PTED who were the learning curve cases performed by surgeons who did not do PTED before the trial.
Interventions PTED (n=179) compared with open microdiscectomy (n=309).
Main outcome measures The primary outcome was self-reported leg pain measured by a 0-100 visual analogue scale at 12 months, assuming a non-inferiority margin of 5.0. Secondary outcomes included complications, reoperations, self-reported functional status as measured with the Oswestry Disability Index, visual analogue scale for back pain, health related quality of life, and self-perceived recovery. Outcomes were measured until one year after surgery and were longitudinally analysed according to the intention-to-treat principle. Patients belonging to the PTED learning curve were omitted from the primary analyses.
Results At 12 months, patients who were randomised to PTED had a statistically significantly lower visual analogue scale score for leg pain (median 7.0, interquartile range 1.0-30.0) compared with patients randomised to open microdiscectomy (16.0, 2.0-53.5) (between group difference of 7.1, 95% confidence interval 2.8 to 11.3). Blood loss was less, length of hospital admission was shorter, and timing of postoperative mobilisation was earlier in the PTED group than in the open microdiscectomy group. Secondary patient reported outcomes such as the Oswestry Disability Index, visual analogue scale for back pain, health related quality of life, and self-perceived recovery, were similarly in favour of PTED. Within one year, nine (5%) in the PTED group compared with 14 (6%) in the open microdiscectomy group had repeated surgery. Per protocol analysis and sensitivity analyses including the patients of the learning curve resulted in similar outcomes to the primary analysis.
Conclusions PTED was non-inferior to open microdiscectomy in reduction of leg pain. PTED resulted in more favourable results for self-reported leg pain, back pain, functional status, quality of life, and recovery. These differences, however, were small and may not reach clinical relevance. PTED can be considered as an effective alternative to open microdiscectomy in treating sciatica.
Trial registration NCT02602093ClinicalTrials.gov NCT02602093.
Introduction
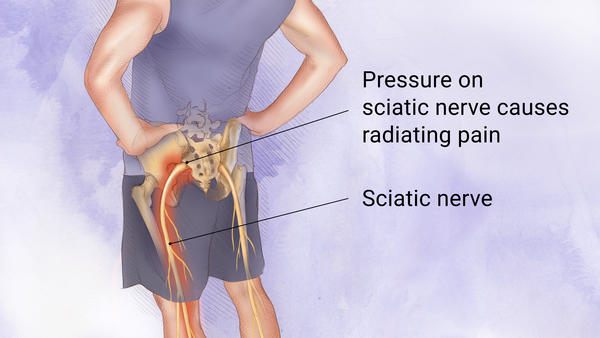
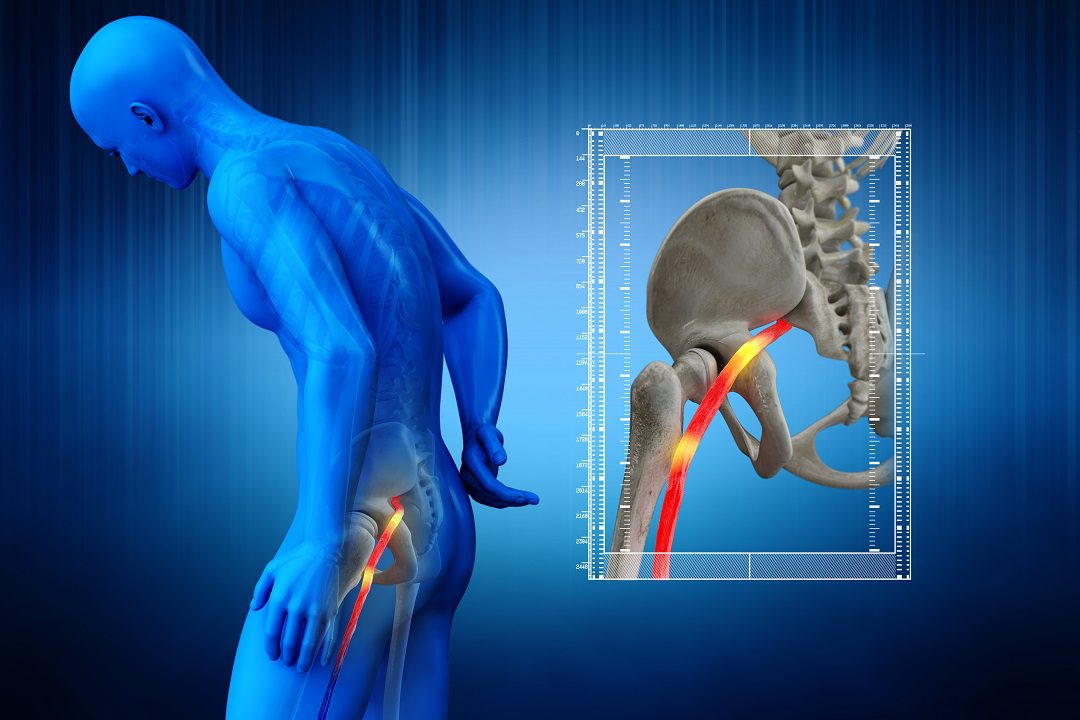
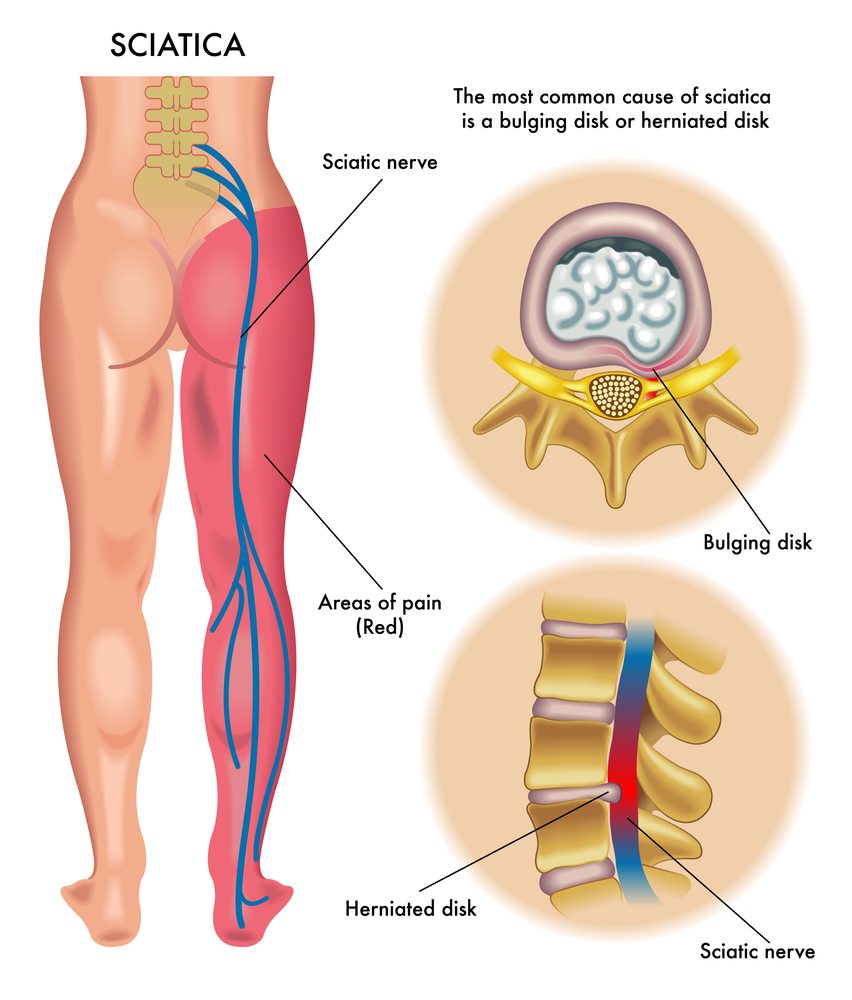
With a lifetime prevalence of up to 43%, sciatica is a common health problem in the general population.1 Sciatica is typically characterised by radiating leg pain starting from the low back, at times accompanied by sensory or motor deficits, and most frequently caused by lumbar disc herniation.23 Sciatica has a favourable natural course in most people; however, surgery may be indicated when conservative treatment fails or progressive neurological deficits develop.4 Previous studies have shown the short term benefits of surgery for pain relief, function, and perceived recovery, with similar long term outcomes to prolonged conservative management for people with sciatica lasting from six to 12 weeks. Recent studies showed that surgery led to a greater reduction in leg pain on long term follow-up compared with conservative management for sciatica lasting from four to 12 months.56
Following publication of initial reports on surgery for lumbar disc herniation in 1934, attempts were made to reduce the surgical invasiveness of this procedure.78 These modifications have led to conventional transflaval open microdiscectomy becoming the standard procedure for treating lumbar disc herniation.910 Owing to the development of surgical endoscopes and their application to the lateral transforaminal “safe” entry zone as described by Kambin and Brager, other surgical techniques were developed with the intention to be less invasive.1112 Percutaneous transforaminal endoscopic discectomy (PTED) is one of these proposed less invasive techniques. PTED is expected to lead to less postoperative back pain, shorter hospital admission, and a faster recovery because paraspinal muscles are not detached from their insertion, bony anatomy is not changed, and general anaesthesia is not used.13 Some concerns exist, however, in the scientific literature about the effectiveness for leg pain and recovery of function after PTED compared with open microdiscectomy, and previously published studies may have been influenced by commercial enterprises.14151617 Furthermore, as PTED has a learning curve and exposes surgeons and patients to a higher radiation dose, these concerns need to be overcome with high quality evidence before PTED can be widely implemented.17181920
Previous studies that have compared PTED with open microdiscectomy found either no differences in outcomes or small differences of uncertain clinical relevance.141516172122 However, these studies were of small sample size, were not randomised, or involved only one surgeon.1415162122 Therefore, a randomised controlled trial with adequate sample size and low risk of bias is warranted. Advantages adherent to minimally invasive surgery are claimed for PTED, such as less postoperative back pain and shorter hospital admission, so we hypothesised that PTED should not be worse than open microdiscectomy in treating leg pain to be offered as a treatment alternative. Therefore, the aim of the PTED-study was to investigate whether the effect of PTED was non-inferior to conventional open microdiscectomy in terms of reduction in leg pain in patients having surgery for sciatica caused by lumbar disc herniation.
Methods
Trial design
This multicentre, non-inferiority randomised controlled trial was conducted at four general hospitals in the Netherlands in patients with sciatica caused by lumbar disc herniation. Details of the protocol and study design have been published previously.23 The study was funded by ZonMw, the Netherlands Organisation for Health Research and Development, without involvement of the medical technology industry. The research protocol was approved by the research ethics board of all participating hospitals and registered at ClinicalTrials.gov (NCT02602093). All patients provided written informed consent before enrolment.
Enrolment and randomisation
From February 2016 to April 2019, neurosurgeons and orthopaedic surgeons screened and enrolled patients with sciatica during outpatient clinic visits. Patients were eligible for the PTED-study if they had an indication for surgery according to Dutch consensus, which means that patients should have at least six weeks of excessive radiating leg pain with no tendency for any clinical improvement despite conservative therapy. Aside from leg pain, patients could be included with or without motor or sensory loss, as is part of daily practice. Furthermore, patients should be between 18 and 70 years of age; have a nerve root compression by a lumbar disc herniation proven by magnetic resonance imaging, corresponding to the clinical dermatomal area; and have sufficient knowledge of the Dutch language to complete forms and follow instructions independently. Exclusion criteria were previous surgery at the same or adjacent disc level; cauda equina syndrome; isthmic or degenerative spondylolisthesis; pregnancy; severe comorbid medical or psychiatric disorder (American Society of Anesthesiologists’ classification >2); severe caudal or cranial sequestration of disc fragments, defined as sequestration towards more than half of the adjacent vertebra; contraindication for surgery, and moving abroad on short notice.
We randomised patients in a one to one ratio to PTED or open microdiscectomy by using computer generated variable block sizes (four, six, or eight), stratified by enrolling centre. Blinding of patients was not feasible because of the substantial differences between the two procedures (for example, PTED being performed under conscious sedation and having an 8 mm incision 8-12 cm lateral of the spine midline and open microdiscectomy being performed under general anaesthesia with a 2-4 cm dorsal incision in the spine midline). Both surgical techniques were presented to patients as equal in effectiveness during enrolment.
Study interventions
All surgeons were spine dedicated with eight to 11 years of experience in degenerative lumbar spine surgery. One of the primary reasons for conducting this study was the opinion that PTED did not meet scientific criteria inherent in reimbursement within the Dutch public healthcare system.24 Therefore, PTED was temporarily reimbursed by insurance companies on the condition that patients were enrolled in the PTED-study. Furthermore, only one of the participating surgeons was proficient in doing PTED in the Netherlands; therefore, three surgeons (one per hospital) were trained to do PTED. Each surgeon attended an accredited postgraduate hands-on workshop and did 10-15 procedures under the supervision of a senior surgeon with ample experience in PTED. After these supervised procedures, the surgeons did PTED independently. Their first 50 cases (including the supervised cases) would be deemed learning curve cases.
PTED
The full procedure has been described previously.13 Local anaesthesia was administered, and surgery was performed under conscious sedation. The site was verified by fluoroscopy, after which a line was drawn from the centre of the herniation. The needle was placed, and the position was checked. After the needle had reached the correct position, a guidewire was inserted. After that, a series of conical rods were introduced, and subsequently a drill was introduced through the cannula. By drilling, the neuroforamen was enlarged. Hereafter, the instruments were removed with the guidewire remaining in place. Then, the endoscope with the working channels was introduced via the cannula. Following removal of the loose disc fragments, the cannula and endoscope were removed. Patients were treated on an outpatient basis.
Open microdiscectomy
Open microdiscectomy was conducted under general anaesthesia.9 The disc level was verified using fluoroscopy, and a paramedian incision was made. The use of loupes or a microscope was optional. After identification of the lamina, the yellow ligament was removed to identify the nerve root and disc herniation. The amount of degenerative disc material removed was at the discretion of the surgeon. Laminotomy, as well as foraminotomy, was done if necessary. A partial medial facetectomy was used for the foraminal herniated disc, and an approach alongside the facet joints was used for the extraforaminal herniated disc. The patient was discharged as soon as medically responsible, which is usually one day after surgery.
Patients in both groups were discharged as soon as medically responsible. Pain medication was offered to all patients if necessary and included paracetamol and optionally non-steroidal anti-inflammatory drugs, short acting opioids, or both. We used questionnaires to monitor the use of pain medication and of co-interventions.
Outcome measures
The primary outcome was the improvement in leg pain at one year, as measured with a visual analogue scale ranging from 0 to 100 with higher scores indicating more leg pain.2526 We chose the visual analogue scale for leg pain as the primary outcome because the goal of surgery is to reduce leg pain, so PTED should be non-inferior in reduction of leg pain to be considered as a treatment alternative to open microdiscectomy. The visual analogue scale for leg pain was measured at baseline; one day; two, four, and six weeks; and three, six, nine, and 12 months postoperatively. Secondary outcomes were functional status as measured with the Oswestry Disability Index (ranging from 0 to 100, with higher scores indicating more disability)27; visual analogue scale for back pain (ranging from 0 to 100, with higher scores indicating more back pain)26; visual analogue scale for quality of life (ranging from 0 to 100, with higher scores indicating a higher quality of life)28; the physical component summary and mental component summary of the short form 36 (SF-36),2930 with higher scores indicating better perceived health; and seven point Likert-type scales measuring self-perceived recovery from symptoms, recovery from leg pain, satisfaction with treatment, and change in symptoms.2829313233 We defined recovery and satisfaction by combining “complete” and “nearly complete” recovery or satisfaction. We added an 11 point numerical rating scale for leg pain, back pain, and quality of life for internal validation of the study results in a protocol amendment.34 All secondary outcome measures were assessed at the same time points as the primary outcome except for one day postoperatively, when only functional disability, quality of life, back pain, self-perceived recovery, and satisfaction were measured. Questionnaires were sent to patients by email or regular mail. At six weeks, three months, and 12 months after surgery, patients visited the clinic for a neurological examination by a research nurse who was aware of the treatment allocation. In addition to the patient reported outcome measures, data on the surgical procedure, complications, discharge, and reoperations were collected. Supplementary table A gives an overview of all outcomes measured in the PTED-study.
Statistical analysis
The expected mean difference between the groups in visual analogue scale for leg pain was 5 with a standard deviation of 14.9.35 With a margin of non-inferiority set at 5.0 (expected difference), a one sided α of 0.05, and a β of 0.10, we estimated that a sample size of 306 patients would show non-inferiority with 90% power. Considering an attrition rate of 20%, we set the sample size at 382. We planned to recruit an additional 150 patients (50 per surgeon) for the learning curve in the PTED arm. We based this decision to include 50 learning curve cases per surgeon on the literature and consensus of the research group.1836 We excluded these learning curve cases from the primary analyses. In total, we included an additional 300 patients (150 randomised to PTED as learning curve cases and 150 randomised to open microdiscectomy) above the sample size calculation because reimbursement of PTED was dependent on participation in the trial. Thus, the goal was to recruit 682 participants.
We did the primary analyses according to the intention-to-treat principle. We did per protocol analyses as sensitivity analyses, including only patients who received the intervention to which they were randomised. Furthermore, we did sensitivity analyses including the learning curve patients and sensitivity analyses using the numerical rating scale to test the robustness and validity of the results. We presented baseline characteristics by using percentages for categorical variables and means and standard deviations or medians and interquartile ranges, when appropriate, for continuous variables. We used mixed model analyses with random intercepts on the patient level to account for dependency of measurements over time within patients. We used linear mixed models to analyse leg pain, functional disability, back pain, quality of life, physical component summary, and mental component summary. We used logistic mixed models to analyse the dichotomised Likert-type scales. In addition to the adjusted models in which we corrected for the baseline score and centre, fully adjusted models for the primary analyses are shown in the supplementary material. Fully adjusted models included adjustment for factors such as the baseline score, centre, age, sex, duration of complaints, smoking status, body mass index, employment status, site of disc protrusion, treatment preference of the patient, and psychopathology as measured on the four dimensional symptom questionnaire.3738 Finally, we added a linear and logistic regression analysis adjusting for baseline and hospital for the outcomes at 12 months as an alternative analysis. Mean differences and odds ratios are presented with their 95% confidence intervals. We estimated confidence intervals from linear mixed model analyses by using 1000 bootstrap samples according to the bias accelerated procedure to take into account skewness of residuals. We used SPSS version 27.0 for all analyses.
As follow-up data were collected using electronic questionnaires, all patients who had data available had complete data available at that follow-up point. We handled data missing owing to missed visits or patients’ withdrawal from the study at follow-up time points by mixed model analysis using the maximum likelihood estimation.
Amendments from original trial protocol
Some amendments were made to the study protocol after enrolment started but before the study was completed. One was the inclusion of an 11 point numerical rating scale for the outcomes that were measured by a visual analogue scale—leg pain, back pain, and quality of life. The reason for this was that some concerns were raised about the validity of the visual analogue scale, as its length may differ while using different electronic devices (for example, smartphone, tablet, or laptop) and we had not standardised the use of one of these devices. We therefore added the numerical rating scale for leg pain as the primary outcome. However, because we expected results of the visual analogue scale and numerical rating scale to be similar, we reinstated the visual analogue scale as the primary outcome. For reasons of transparency, we also report the results for the numerical rating scale on the primary outcome, leg pain, as a sensitivity analysis. Secondly, we increased the enrolment period of the trial by one year. Before the trial started, we had planned to recruit patients during a two year period. Because the enrolment was slower than anticipated, we increased the enrolment period to three years. Finally, we increased the follow-up period of the included patients to also include 24 month and 60 month measurements.
Patient and public involvement
Before the start of the PTED-study, members of the patients’ organisation “de Wervelkolom” (“the Spine”) were involved in the study design. Furthermore, this organisation was also part of the half yearly board meetings during which recruitment, implementation, and results of the study were discussed. The general public was not involved with the study.
Results
Patients
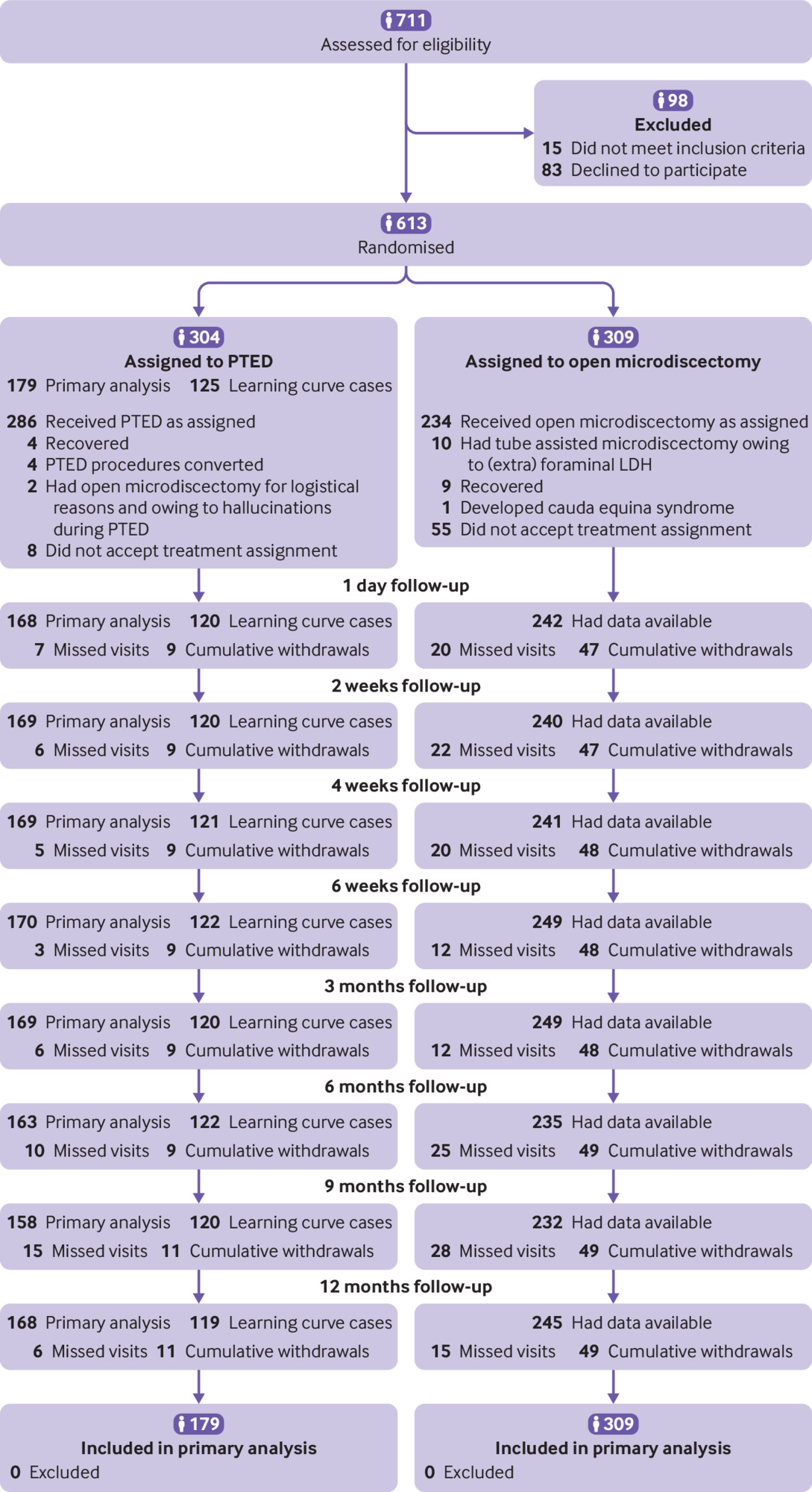
In the period between February 2016 and April 2019, 711 patients were assessed for eligibility, of whom 613 patients were enrolled into the PTED-study (fig 1). The baseline characteristics of the patients were similar in both groups (table 1). The trial was finalised before the estimated sample size of 682 participants was reached, because the end of the enrolment period of the study was reached. Of the 304 patients randomised to PTED, 286 (94%) received the intervention; of the 309 patients randomised to open microdiscectomy, 244 (79%) had microdiscectomy as assigned; 10 of these were tube assisted. At 12 months of follow-up, the primary outcome was available for 532 (87%) of the randomised patients.

Flowchart of study eligibility, enrolment, procedures, and outcomes. LHD=lumbar disc herniation;PTED=percutaneous transforaminal endoscopic discectomy
Characteristics of participants. Values are numbers (percentages) unless stated otherwise
Learning curve
The estimated learning curve of 150 learning curve cases was not reached. Of the 304 patients randomised to the PTED group, 125 were learning curve cases (supplementary table B). During the learning curve, the PTED procedure was converted to open microdiscectomy in four patients (supplementary table C). Four complications occurred, and 14 (11%) patients had repeated surgery within one year because of recurrent disc herniation. All patient reported outcome measures showed significant improvement after 12 months (supplementary table C) compared with baseline.
Primary outcome
The median visual analogue scale for leg pain showed a similar improvement in leg pain in both groups following surgery (fig 2). In the first three months, mean differences in reduction of leg pain between the groups were small (table 2; supplementary table D). At six, nine, and 12 months, mean differences in favour of PTED increased. At 12 months’ follow-up, the mean between group difference in leg pain was 7.1 (95% confidence interval 2.8 to 11.3) in favour of PTED. This between group difference indicates that PTED was non-inferior, because the between group difference in leg pain was not worse than 5.0 at 12 months for PTED compared with open microdiscectomy.

Median scores on visual analogue scale for leg pain, Oswestry Disability Index, visual analogue scale for back pain, visual analogue scale for quality of life, SF-36 physical component summary, and SF-36 mental component summary. PTED=percutaneous transforaminal endoscopic discectomy
Primary and secondary outcomes according to treatment and timing of treatment after surgery
Secondary outcomes
In general, mean differences in secondary outcomes between both groups were small in the first three months and increased in favour of PTED at six, nine, and 12 months (fig 2; table 2). At 12 months, the median score on the Oswestry Disability Index was 10.0 (interquartile range 2.0-17.8) in the PTED group and 12.7 (2.2-28.4) in the open microdiscectomy group (mean difference of 5.3, 3.0 to 7.7). At 12 months, back pain intensity was 16.0 (interquartile range 3.0-38.8) in the PTED group compared with 21.0 (5.0-55.0) in the open microdiscectomy group (mean difference 6.0, 2.0 to 10.0). Furthermore, at 12 months the median visual analogue scale score for quality of life was 76.5 (interquartile range 61.8-86.8) in the PTED group compared with 70.5 (54.3-83.0) in the open microdiscectomy group (mean difference of −6.2, −9.2 to −3.2). The mean differences for the SF-36 physical component summary and mental component summary at 12 months were in the same direction as the other secondary outcomes: −2.8 (−4.1 to −1.6) and −2.1 (−3.4 to −0.9), respectively. At 12 months, the odds ratio for recovery of symptoms was 2.7 (95% confidence interval 1.4 to 5.2), and the odds ratio for recovery of leg pain was 2.0 (1.0 to 3.7). Furthermore, the odds ratio for satisfaction with change in symptoms and satisfaction with the result of treatment were 2.6 (1.4 to 4.8) and 2.6 (1.3 to 5.0), respectively.
Complications and surgical outcomes
Both procedures were of similar duration, but less perioperative blood loss occurred in the PTED group (table 3). Eight (3%) dural tears and three (1%) wound infections were reported in the open microdiscectomy group compared with none in the PTED group. One (0.4%) nerve root injury and one (0.4%) deep vein thrombosis occurred in the open microdiscectomy group. Of the patients in the PTED group, 94% could be discharged on the day of surgery compared with 6% in the open microdiscectomy group. Measured at six weeks, the mean length of the scar was 11.7 (SD 9.2) mm in the PTED group and 38.4 (15.0) mm in the open microdiscectomy group. The rate of repeated surgery within one year was 5.3% in the PTED group compared with 5.6% in the open microdiscectomy group. At two weeks and six months of follow-up, the use of non-opioid analgesics seemed to be similar between both groups, whereas patients in the PTED group seemed to use fewer non-opioid analgesics at 12 months than did patients in the open microdiscectomy group. Furthermore, patients from the PTED group used fewer opioid analgesics than did patients from the open microdiscectomy group at two weeks, six months, and 12 months of follow-up.
Surgical outcomes and complications of patients who had surgery, according to intention-to-treat analysis. Values are numbers (percentages) unless stated otherwise
Alternative, per protocol, and sensitivity analyses
Figure 3 gives an overview of all analyses conducted for the primary outcome. In general, all alternative analyses did not significantly affect the main results. The results of the alternative analyses using linear regression shows a between group difference of 7.9 (1.8 to 13.4) in favour of PTED on the visual analogue scale for leg pain at 12 months (supplementary table E). The per protocol analysis included 168 patients who had PTED and 244 patients who had open microdiscectomy (supplementary tables F and G). At 12 months, the mean between group difference in improvement of leg pain for PTED compared with open microdiscectomy was 8.3 (4.1 to 12.8). Secondary outcomes were also comparable to the results according to the intention-to-treat analysis. In addition, we did sensitivity analyses including the 125 learning curve cases of all three surgeons who did not do PTED before the study. These analyses resulted in comparable outcomes to the primary analysis (supplementary table H). Finally, when we re-ran the analyses using the numerical rating scale instead of the visual analogue scale for leg pain, back pain, and quality of life (supplementary table I), we found similar results to those with the visual analogue scale. The numerical rating scale for leg pain showed a mean between group difference of 0.6 (0.2 to 1.1) at 12 months in favour of PTED.

Results of primary outcome for main and alternative analyses. Mean difference between groups is shown on visual analogue scale (VAS) for leg pain at 12 months, together with 95% confidence interval (CI). Modified intention-to-treat population included all patients randomised to percutaneous transforaminal endoscopic discectomy (PTED) or open microdiscectomy (OM) without learning curve cases. Per protocol population included all patients randomised to PTED or OM who received allocated treatment. Learning curve cases were also omitted for these analyses. Results of modified intention-to-treat population are also presented including learning curve cases. Crude analyses were adjusted for baseline and centre. Fully adjusted analysis included adjustment for baseline score, centre, age, sex, duration of complaints, smoking status, body mass index, employment status, site of disc protrusion, treatment preference of patient, and psychopathology as measured on four dimensional symptom questionnaire
Discussion
In this multicentre trial among patients with sciatica caused by lumbar disc herniation, we found PTED to be non-inferior to open microdiscectomy in reduction of leg pain at 12 months. Mean differences in leg pain reduction between the groups were small in the first three months, but they increased in favour of PTED at six, nine, and 12 months. Different hypotheses can be formulated to explain this difference. An explanation may be that three months after surgery the formation of scar tissue may limit the patients in the open microdiscectomy group more than those in the PTED group, as a less invasive surgical route was used to access the disc herniation. Eventually at 12 months, patients in the PTED group experienced a larger reduction in leg pain than did patients in the open microdiscectomy group, which is a larger difference than expected and clearly within the non-inferiority margin. One can argue as to whether this difference of 7.1 on a 0-100 visual analogue scale would be clinically relevant, as it is below commonly recognised minimally clinically important difference thresholds.3940 Similarly, the secondary patient reported outcomes showed more favourable results for the patients in PTED group—namely, in functional disability, back pain, quality of life, and self-perceived recovery. These effect sizes, however, were small and may also not reach clinical relevance.40 Further results show that the rate of repeated surgery within one year due to sciatica was similar. Analysis of the learning curve cases showed that PTED can safely be adopted by surgeons in different centres under initial supervision of a surgeon proficient in PTED.
Comparison with other studies
A recently published meta-analysis compared PTED with open microdiscectomy in the treatment of sciatica.17 This meta-analysis included 14 prospective studies, of which nine were (quasi)randomised, and eventually concluded that moderate quality evidence existed for no difference in leg pain reduction or functional status at long term follow-up. The results of our study are in line with these findings. Most of the studies in the meta-analysis did not have an adequate randomisation procedure. Three of the identified studies in the meta-analysis had a low risk of selection bias but had some form of attrition or reporting bias.162241 These studies, however, were either underpowered to detect small differences between groups or were conducted by a single surgeon or in single centre. Furthermore, these studies did not show the feasibility of implementing PTED among surgeons naïve to the procedure.
Strengths and limitations of study
Some limitations have to be acknowledged. Firstly, participation bias cannot be ruled out because a proportion of patients with a strong preference for PTED who were randomised to open microdiscectomy dropped out of the study immediately. Secondly, blinding of patients was not possible owing to the substantial differences between PTED and open microdiscectomy. Thirdly, the pre-estimated sample size of 682 patients was not reached. Of the 382 patients calculated as being necessary in the final sample size of the trial (that is, excluding learning curve cases), we were able to include 179 instead of 191 of the patients who would have PTED. However, the sensitivity analysis including the learning curve patients (n=613) confirms the robustness of our findings. Another concern that was raised during the trial related to the validity of the visual analogue scale when used on different electronic devices, as its length may vary. Therefore, during the trial, we added the numerical rating scale as an updated primary outcome instead of the visual analogue scale. However, after looking at the visual analogue scale on different devices, we found that the visual analogue scale always remained as a scale from 0 to 100, no matter the length of the scale on the device. Therefore, we decided, during the trial, to keep the visual analogue scale as the primary outcome and to analyse the numerical rating scale as a sensitivity analysis. Our main analysis shows a between group difference of 7.1 on the 0-100 visual analogue scale for leg pain, which is comparable to the between group difference of 0.6 on the 0-10 numerical rating scale for leg pain. Another point of discussion could be the use of mixed models for our primary analysis. Mixed model analyses adjust the primary outcome at 12 months for leg pain measured at earlier time points and may lead to a subtly different outcome than our defined primary outcome of improvement in leg pain at 12 months. Both methods of analysing the data (linear regression and mixed model) suggest similar outcomes (fig 3; supplementary table E) and support the conclusion that PTED is non-inferior to open microdiscectomy in leg pain reduction.
Strengths of this study include the multicentre, randomised design and the inclusion of learning curve cases in the sample size. An additional strength is the generalisability. We chose the study’s inclusion and exclusion criteria to reflect current neurosurgical practice for sciatica. This is also underlined by the proportion of patients that were enrolled after screening. Another strength is the signed agreement on the non-inferiority margin by the research group, patients’ organisation, professional organisations and the Dutch Health Care Institute, before the trial started. Furthermore, clinical outcomes, complications, and adverse events were structurally documented between short time intervals.
Policy implications
Before this study, PTED was not reimbursed by various insurance companies because of the lack of evidence on the benefits of PTED compared with open microdiscectomy in the treatment of sciatica. The results of the study show that PTED is non-inferior to open microdiscectomy in the treatment of leg pain but also that no meaningful clinical differences in patient reported outcomes exist between the procedures. Therefore, future decisions on doing lumbar discectomy should consider patients’ preferences for a treatment, the burden of the treatment to the patient, and the costs of the treatment. Aside from the lack of clinically relevant differences between the procedures, PTED comes with advantages of facilitating outpatient surgery, less estimated blood loss, a low complication rate, lower use of opioids, and a smaller scar, as well as a comparable rate of repeated surgery within one year. Furthermore, 81% of the patients included preferred PTED, indicating the popularity of this procedure among patients. PTED, however, has a learning curve with a higher rate of repeated surgery within one year, more exposure to perioperative radiation, and possibly greater costs.171920 Whether the small differences in clinical outcomes and the advantages of PTED will outweigh the potential higher costs of the procedure remains open for debate. To answer these remaining questions, an economic evaluation has been conducted alongside the PTED study and is being published separately.42 As a result of this study, the Dutch government now reimburses PTED and patients are able to have PTED outside of the experimental setting. This reimbursement also comes with the need for an implementation plan to ensure that the PTED technique is performed by surgeons who have received proper training.
Conclusions
PTED was non-inferior to open microdiscectomy in reduction of leg pain. PTED resulted in more favourable results for patients’ self-reported leg pain, back pain, functional status, quality of life, and recovery. These differences, however, were small and may not reach clinical relevance. PTED can be considered as an effective alternative to open microdiscectomy in treating sciatica.
Acknowledgments
We gratefully acknowledge the support of the Dutch Health Insurance Board; ZonMw, the Netherlands Organisation for Health Research and Development; the participating patients; the patients’ organisation de Wervelkolom (nvvr); Pieter J Schutte (Alrijne Hospital) and Arnold Vreeling (Rijnstate Hospital) as study surgeons; and the research nurses Esther Willemsen, Steffi van Beek, Chantal Ritskes, Monique Stuit (Park MC), Paula van Limpt (Elisabeth-TweeSteden Hospital), Moniek Vroemen, Annemiek Hol (Rijnstate Hospital), and Marjon Nuijten (LUMC, Alrijne Hospital).

We understand how important it is to choose a chiropractor that is right for you. It is our belief that educating our patients is a very important part of the success we see in our offices.