

The familiar twinge in your lower back. A sensation that establishes itself more firmly with each passing year. But have you ever stopped to wonder why?...


Ciática, un término que suele resonar en los pasillos de la atención médica, se refiere al dolor que se irradia a lo largo del nervio ciático....


Muscle pain can be a relentless companion, whether from an intense workout, a long day of physical labor, or the stresses of daily life catching up...


Are you seeking a gentler approach to sciatica pain management? Let’s find out how effective are herbal supplements for alleviating sciatica pain. People have used herbal...

Sciatica can be a real pain in the back. Literally. The affected area of pain in sciatica can vary widely, often affecting the hip bone and...


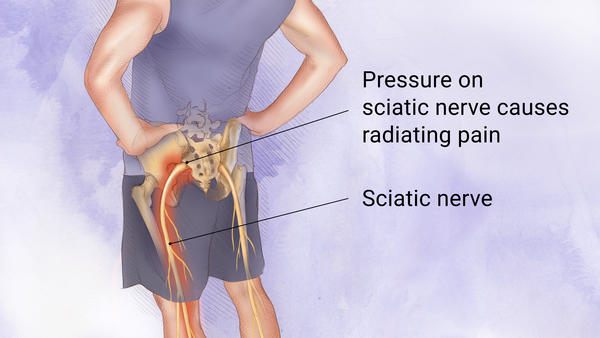
Sciatica, a term often resonating in the corridors of healthcare, refers to pain radiating along the sciatic nerve. This nerve runs from the lower back, through...


Sciatica nerve pain is one of the most common forms of chronic lower back pain. It is typically caused by a pinched sciatic nerve, which can...
Sciatica is a painful condition that affects the sciatic nerve and can cause intense pain in the lower back, buttocks and legs. It is important to...
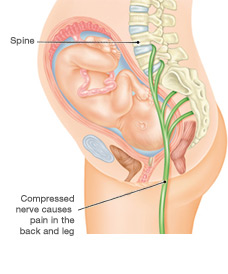
Sciatica is a type of back pain that can occur during pregnancy. It is caused by an irritation or compression of the sciatic nerve which runs...

Sciatica is a common form of lower back pain. It can be caused by inflammation or compression of the sciatic nerve, which runs from the pelvis...