La ciática es una condición frustrante que puede causar mucho dolor. Para los corredores, la pregunta es: ¿correr agravará la ciática? La respuesta corta es que...
La ciática es una afección común que puede causar dolor en la parte baja de la espalda y las piernas. El dolor es causado por la...
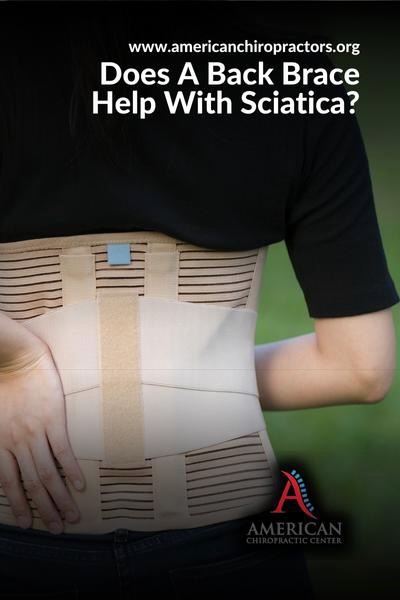
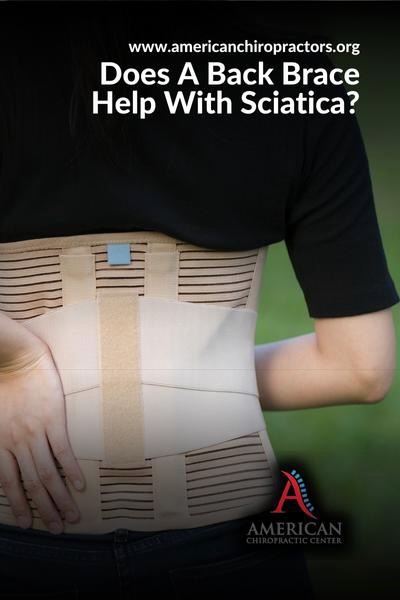
Sciatica is a common condition that can cause pain in the lower back and legs. The pain is caused by pressure on the sciatic nerve, which...


Sciatica is a frustrating condition that can cause a great deal of pain. For runners, the question becomes: will running aggravate sciatica? The short answer is...


A common question that patients with arthritis and sciatica ask is whether or not there is a connection between the two conditions. While it is true...
If you’ve been diagnosed with a pilonidal cyst, you may wonder how painful it is and how long it will take to go away. You may...
La ciática es un dolor común que afecta a millones de personas cada año. La afección es causada por la compresión del nervio ciático, que se...
La ciática es una dolencia dolorosa que puede causar entumecimiento y hormigueo en las piernas y la espalda baja. La causa exacta del dolor no está...
La ciática es una afección común que causa dolor en la parte baja de la espalda y las piernas. Varias cosas, como una hernia de disco...
Sciatica is a common condition that causes pain in the lower back and legs. Various things, such as a herniated disc or spinal stenosis, can cause...