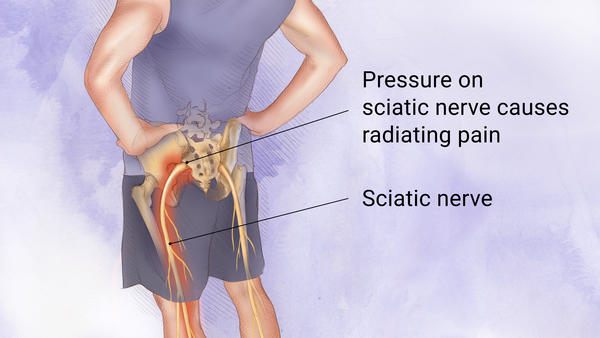
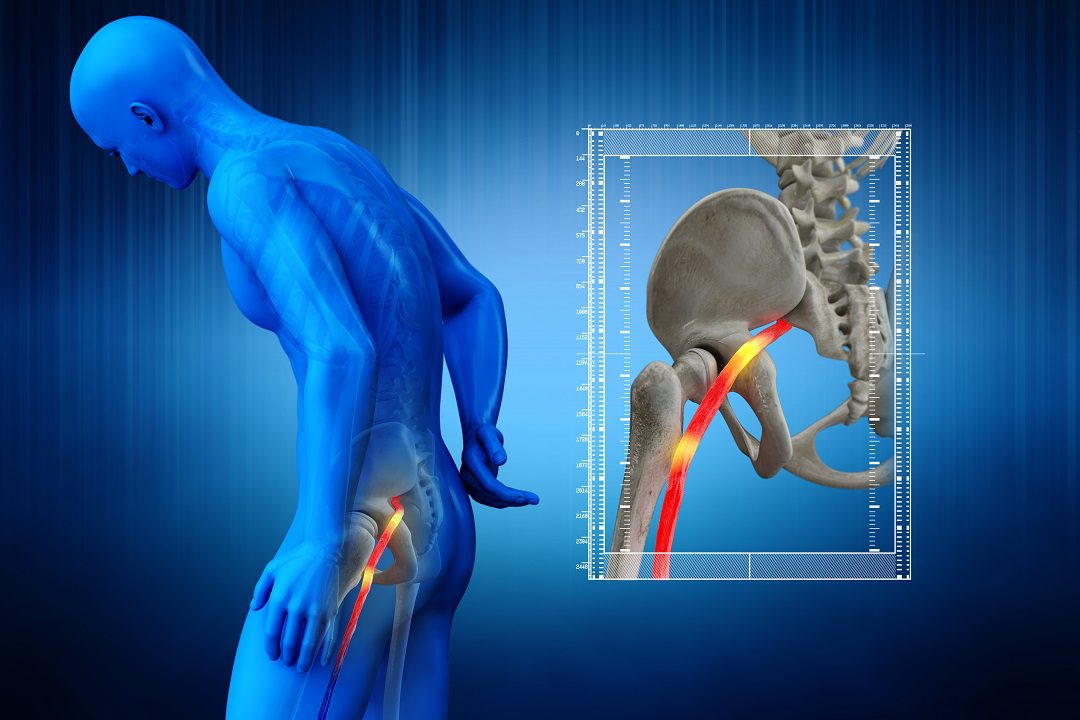
Sciatica
Nass 2022: Transforaminal percutaneous discectomy, a less expensive treatment option than microdiscectomy for sciatica (see below). Spinal News International

The percutaneous transforaminal endoscopic diskectomy (PTED) is cheaper from a societal standpoint at 24 months than microdiscectomy for patients suffering from sciatica. This is based on studies presented during the North American Spine Society’s (NASS) annual meeting (12-15 October, Chicago, USA) by Pravesh Gadjradj (Weill Cornell, Brain and Spine Centre, New York, USA) and was awarded the Value Award winner.
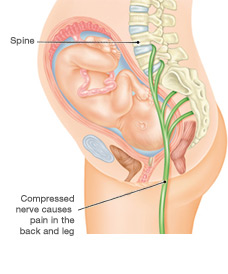
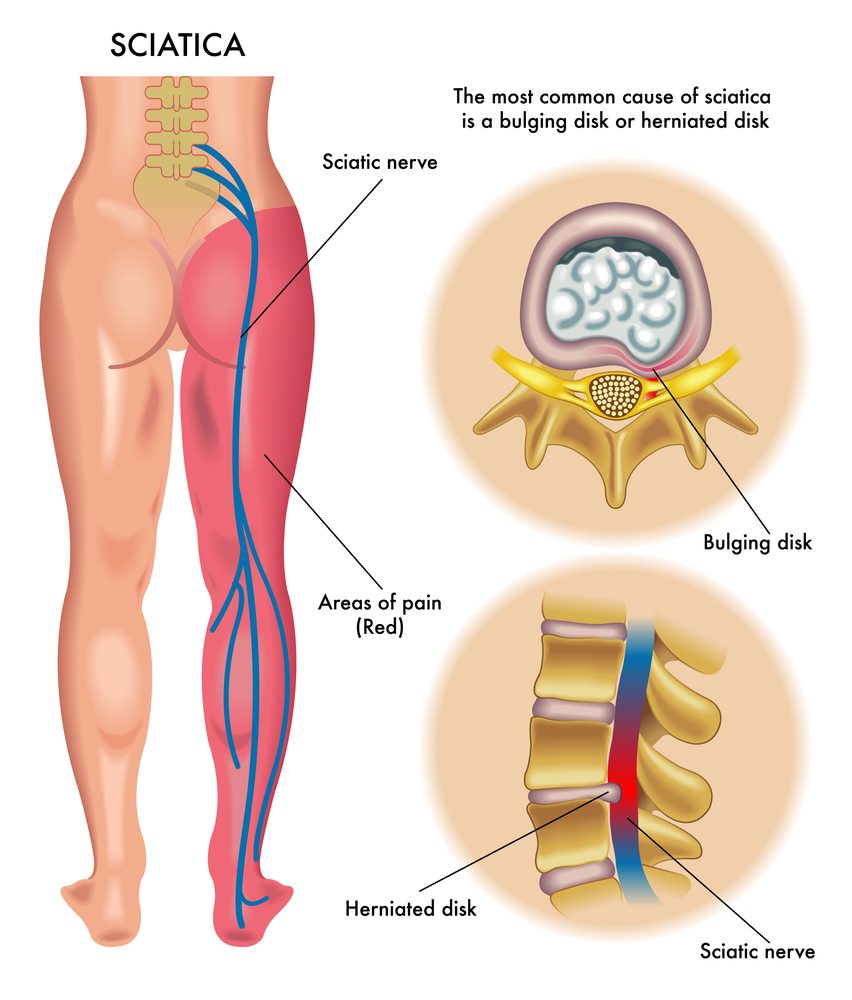
Microdiscectomy is a commonly performed surgical procedure that treats sciatica caused by disc herniation in the lumbar region. But, PTED has been introduced as a less invasive option and results over two years demonstrate non-inferiority in reducing leg pain and superiority in cost-effectiveness, says Gadjradj.
This particular controlled, randomised trial was carried out at 4 clinics across the Netherlands and was conducted from February 2016 until April 2019. Patients ranged in age between 18 and 70 and suffered at minimum six weeks of leg pain due to the herniation of the lumbar disc.
The trial comprised an established group comprising 125 PTED patients, who were first cases to be performed by 3 surgeons that had never previously performed PTED prior to the trial. The trial concluded that 304 patients were allocated the procedure of PTED and 309 were assigned to open microdiscectomy.
The main effect measures were leg pain, as measured by the Visual Analogue Scale (VAS) and health-related quality of living (QALYs). Costs were evaluated from a social view.
At the 24 month time frame after 24 months, 92% of follow-up information were available. The results demonstrate statistically significant variations in leg pain and QALYs with PTED after the age of 24 (leg discomfort: 7.3; QALYs: 0.043).
Surgery costs were demonstrated to be greater for PTED than open-microdiscectomy (EUR4,500 per patient as compared to. EUR4,095 for each patient). But, the other disaggregated costs, as well as the total social costs decreased for PTED as compared to open microdiscectomy. This includes primary health care, secondary healthcare medications and informal care, absenteeism as well as presenteeism and productivity loss.
Additionally, EUR138 in health care costs and EUR2,787 for societal expenses were saved with each PTED procedure that was performed. Cost-effectiveness acceptability curves revealed that the chance of PTED being cost effective compared to open microdiscectomy (meaning that it is on average less expensive and more efficient) was 99.4 percent for leg pain, and 99.2 percent for QALYs regardless of willingness to pay.
In an interview with Spinal News International, Gadjradj said: “Previously we have demonstrated the non-inferiority effect of PTED in the reduction of leg pain when compared to microdiscectomy just within one year of surgery. While we have demonstrated the advantages of microdiscectomy, there were some concerns nevertheless raised about its long-term efficacy and especially the possibility of recurrent surgery.
“In the present study, we address these concerns by showing the non-inferiority of PTED in the reduction of leg pain and its superiority in cost-effectiveness two years following surgery. I would like to see these findings inspire surgeons to think about offering full-endoscopic procedures more often to treat sciatica.”

We understand how important it is to choose a chiropractor that is right for you. It is our belief that educating our patients is a very important part of the success we see in our offices.